Many people wonder if multiple sclerosis (MS) runs in families or is inherited from parents.
MS is not directly passed from parent to child, but having a family member with MS can raise a person’s risk a little.
So, even though it isn’t considered an inherited disease, family history does play a role in risk.
There are over 200 genes that might affect someone’s chances of getting MS, but genetics is just one piece of the puzzle.
Other factors, like environment, lifestyle choices, and immune system issues, also have an impact.
To truly understand your risk, it’s important to look at the whole picture—not just family history.
Key Takeaways
- MS is not directly inherited from parents.
- Both genetic and non-genetic factors affect MS risk.
- Diagnosis and long-term outlook depend on many different influences.
What Is Multiple Sclerosis?
IN THIS ARTICLE

Multiple sclerosis (MS) is a lifelong condition that affects the brain and spinal cord.
It is considered an autoimmune disorder, which means the body’s immune system attacks its own tissues, damaging the protective covering of nerve fibers known as myelin.
Characteristics of Multiple Sclerosis
MS is marked by inflammation and demyelination in the central nervous system. Damage mainly affects nerve fibers in the brain and spinal cord.
The loss of myelin disrupts how electrical signals travel along the nerves. This can slow down or block messages between the body and the brain.
Multiple sclerosis often involves periods where symptoms get worse, called relapses, and periods of recovery.
Over time, some people develop permanent nerve degeneration. This can lead to gradual disability, mobility problems, and changes in coordination or memory. The severity and speed of progression are different for each person.
MS is not a contagious or inherited disease, although genetics may play a role in risk. The inflammatory response seen in MS comes from the immune cells attacking healthy tissue by mistake.
Types of Multiple Sclerosis
There are several distinct forms of MS.
The most common type is relapsing-remitting multiple sclerosis (RRMS). People with RRMS experience clear relapses followed by partial or full recovery periods. Symptoms may disappear in between attacks but can become more severe with each relapse.
Another type is secondary-progressive multiple sclerosis (SPMS). With SPMS, symptoms worsen steadily over time, with or without relapses or remissions. Early RRMS can transition into SPMS.
Primary-progressive multiple sclerosis (PPMS) is less common and is marked by a gradual worsening of symptoms from the start, without relapses or remissions. Each type varies in its rate of nerve damage, progression of disability, and response to treatments.
Common Symptoms
MS symptoms depend on which nerves are affected. Common problems include fatigue, numbness, tingling, and weakness in limbs. Many people experience vision problems such as double or blurred vision.
Muscle issues like weakness, spasticity, double vision, and poor coordination are common. Bladder problems can also occur, such as frequent or urgent urination. Some may have trouble with memory, attention, or cognition.
MS can also lead to chronic pain, balance problems, and changes in mood. Because it is a neurodegenerative disease, symptoms can vary widely and may get worse over time.
For more on these symptoms, visit the Mayo Clinic’s overview of MS symptoms and causes.
Hereditary and Genetic Factors in Multiple Sclerosis
Multiple sclerosis (MS) is not inherited directly, but genetics can still raise a person’s risk.
Having a close family member with MS can make it more likely, and certain gene changes have been linked to this condition.
Overview of Genetic Risk
MS is a complex disease caused by a mix of genetic and environmental factors. It is not a straightforward genetic condition like some inherited diseases. Instead, many different genes may slightly increase a person’s risk of developing MS.
People with MS often have family members with other autoimmune diseases, such as type 1 diabetes or rheumatoid arthritis. Studies show that having a first-degree relative (like a parent or sibling) with MS raises the risk, but it is still much lower than typical genetic diseases.
For most people, the absolute chance of getting MS remains low, even with a family history.
Research suggests that certain populations and ethnic groups are more likely to get MS due in part to genetics. Environmental factors, like where a person lives and their vitamin D levels, can also play a role in addition to their DNA.
Family History and Inheritance Patterns
MS is not classified as an inherited disease. It does not get passed down in a predictable pattern from parents to children, seen in some genetic conditions. This means that if one family member has MS, it does not guarantee others will get it.
However, MS does run in families at higher rates than in the general population. Siblings or children of a person with MS have a slightly higher risk of developing the disease.
The risk is about 2-4% for close family members, compared to about 0.1% in the general population. Even so, most people with MS do not have a family history of the disease.
Factors like gender also seem to matter. MS is more common in women, and the risk patterns can vary between men and women in the same family. Cases can also appear in families with a history of other autoimmune diseases.
Genes Associated With Multiple Sclerosis
MS has been linked to several genes that help the immune system work.
The most well-known is the HLA-DRB1 gene, which plays a role in how the body recognizes its own cells.
Variations in this and other immune-related genes can make the immune system more likely to attack the body’s own nerve fibers, which is what happens in MS. But these gene changes only increase risk—they do not cause MS by themselves.
Researchers have also found links between MS and genes connected to other autoimmune diseases, like type 1 diabetes.
However, having this genetic architecture does not mean someone will definitely develop MS. Genetic risk is just one factor.
Environmental and Lifestyle Influences

Environmental and lifestyle factors have a strong impact on the risk of developing multiple sclerosis.
Specific environmental risk factors include low vitamin D, lack of sunlight, geography, and exposure to certain viruses.
Role of Vitamin D and Sunlight Exposure
Low levels of vitamin D have been linked to a higher risk of multiple sclerosis.
Vitamin D is mostly produced in the skin through sunlight exposure. People who spend more time indoors, or who live in places with little sunlight, may have a higher chance of vitamin D deficiency.
Studies show that taking vitamin D or vitamin D3 supplements may help lower MS risk, especially for those with little sun exposure. Evidence also suggests that children and young adults who get enough sunlight or have higher vitamin D blood levels are less likely to develop MS.
Other environmental factors like smoking and past infection with the Epstein-Barr virus can also increase MS risk. A healthy lifestyle goes a long way.
However, vitamin D and sunlight are among the most researched lifestyle risk factors for this disease (learn more about lifestyle and environmental factors in MS).
Geographical Patterns and Regional Risk
The risk of MS is not the same everywhere. It is much higher in regions farther from the equator. In places like the northern United States, Canada, and parts of Europe, rates of MS are higher compared to regions closer to the equator.
Scientists think this pattern is linked to less sunlight and lower vitamin D levels in these areas. A table can help show the pattern:
| Region | MS Risk Level |
|---|---|
|
Northern United States |
High |
|
Canada & Northern Europe |
High |
|
Tropical regions |
Low |
These geographical differences also suggest that sunlight exposure, and not just genetics, plays a major role in MS risk (read about geographical risk factors for MS).
Autoimmune Mechanisms and Disease Triggers
Multiple sclerosis (MS) happens when the body’s immune system starts attacking nerve cells. As a result, inflammation and nerve damage occur, which affects movement, feeling, and other body functions.
Immune System Dysfunction
In MS, the immune system mistakes healthy tissue for threats. It mainly targets myelin, the protective covering that surrounds nerves in the brain and spinal cord. This response is what makes MS an autoimmune disorder. Scientists believe both genetic and environmental factors play a part.
Family history can increase a person’s risk, but MS is not passed directly from parent to child. People who have relatives with MS have a higher chance of developing it, yet most people with MS do not have a close family member with the disease. The genetic link is complex and no single gene causes MS.
The immune attack leads to long-term nerve problems. MS is more common in young adults and is seen more often in women than men.
Inflammation and Demyelination
The body’s immune response causes inflammation, which damages myelin. This process is called demyelination. Damaged myelin can slow down or block messages between the brain and the rest of the body.
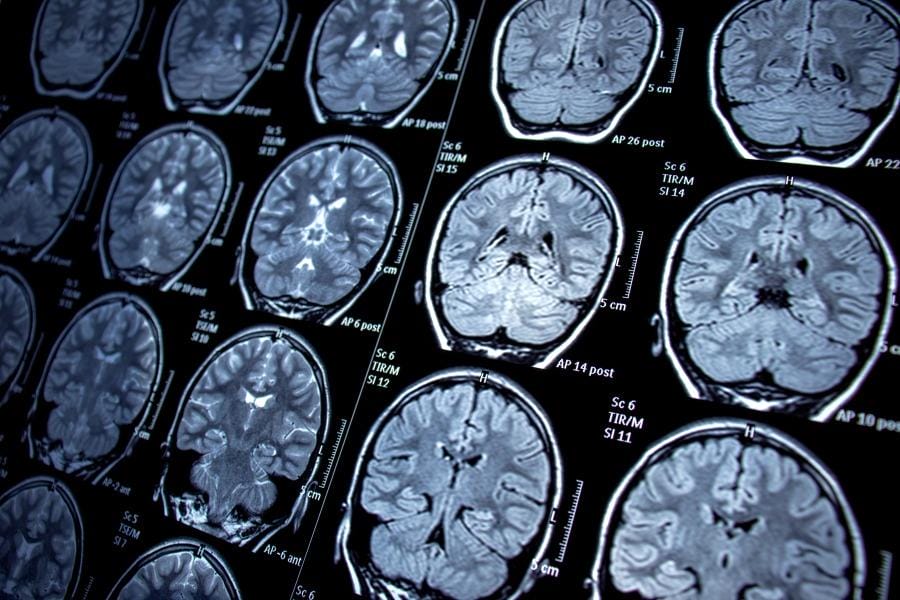
Nerve fibers (axons) might also get harmed, not just the myelin. Patchy areas of damage—called lesions or plaques—form in the central nervous system. These lesions often show up on brain scans.
Inflammation and demyelination can change how a person moves, feels, and thinks.
Symptoms might include:
- Muscle weakness
- Vision problems
- Numbness
- Balance issues
Over time, the damage can build up and cause more disability. MS symptoms can come and go, or keep getting worse depending on the amount and location of nerve damage.
Diagnostic Methods for Multiple Sclerosis
Doctors use several tests to identify multiple sclerosis (MS). No single test can confirm MS, so a mix of methods is needed to look for signs in the central nervous system (CNS) and rule out other conditions.
Neurological Examination and MRI
A neurological examination is usually the first step. The doctor checks for signs of damage in the CNS by testing strength, reflexes, vision, coordination, and balance.
These tests can find problems even if a person does not notice symptoms yet.
Magnetic resonance imaging (MRI) is the main imaging tool for MS. It creates clear images of the brain and spinal cord. MRI can reveal lesions or scars caused by MS, even when there are no clear signs.
Doctors look for specific patterns of lesions in the CNS that are typical for MS. More on the MRI process is explained by the Mayo Clinic.
Lumbar Puncture and Cerebrospinal Fluid Analysis
A lumbar puncture, also called a spinal tap, involves taking a small sample of cerebrospinal fluid (CSF) from around the spinal cord. This test helps find changes linked with MS that cannot be found with MRI alone.
Doctors look for bands of proteins called oligoclonal bands and signs of inflammation. These results, when seen with symptoms and MRI findings, can support an MS diagnosis. Not all people with MS have positive CSF findings, but it is still a helpful step in many cases.
Blood Tests for Differential Diagnosis
Blood tests help rule out other illnesses that have symptoms like MS. They do not diagnose MS, but they are important for excluding infections, inflammatory diseases, and vitamin deficiencies.
Doctors might check for antibodies linked with other autoimmune conditions or look for markers of diseases like Lyme disease or lupus. By using these blood tests, doctors can make sure the symptoms are not caused by another condition. This multi-step approach helps improve the accuracy of diagnosing multiple sclerosis.
Impact on Daily Life and Long-Term Outlook

Multiple sclerosis affects people in many different ways, often impacting their ability to work, move, and think clearly. Over time, symptoms may change or become more noticeable, shaping a person’s routine and future plans.
Living With Multiple Sclerosis
Many people with multiple sclerosis (MS) face daily symptoms such as fatigue, muscle weakness, or trouble with coordination. These symptoms can make it harder to keep up with normal activities like walking, working, or household tasks.
Using mobility aids, home modifications, and personal routines can help people manage physical challenges. Physical therapy, stretching, and low-impact exercise often improve movement and balance. It is important for people to listen to their bodies and ask for help when needed.
Doctors may recommend coping skills for managing unpredictable fatigue. Planning breaks, keeping a regular sleep schedule, and breaking tasks into smaller steps are useful tips. Medications are sometimes prescribed to reduce symptoms or slow the disease.
Disability and Disease Progression
MS can cause varying degrees of disability over time. Some people experience mild symptoms for many years, while others may need mobility devices sooner.
Disability happens mostly because of increasing weakness in the muscles, poor balance, or reduced coordination, especially in the legs. Symptoms often come and go, but they can slowly get worse as the nervous system is affected.
A person’s outlook depends on the type of MS, how fast it progresses, and how early treatment begins. Regular monitoring and updated treatment plans are important in managing long-term effects.
Emotional and Cognitive Challenges
Living with MS often brings emotional changes such as depression and anxiety. Many people struggle with uncertainty and worry about disease flare-ups or losing their independence.
Cognitive issues—like memory loss, slow thinking, and trouble concentrating—are also common. These challenges can be frustrating and may affect work or relationships.
Support from mental health professionals, family, and support groups helps people manage stress and keep a positive outlook. Common treatments include counseling, medication for depression, and brain exercises to support memory and thinking.
Get Premier Nursing Care Today
If a loved one in your life is suffering from MS, NurseRegistry can help.
We supply professional and caring private nurses who can assist with both daily living tasks along with medical care needs.
We take the time to expertly match these healthcare professionals with your loved one based on personality, age, gender, and skill set.
Click below to discover how NurseRegistry can benefit your loved one suffering from multiple sclerosis today.
People Also Ask About MS and Genetic Factors
Multiple sclerosis is not inherited in a simple way, but genes can increase a person’s chances of getting the condition.
Family history and certain genetic factors play a part, but environment and lifestyle also matter.
Can family history affect the likelihood of developing multiple sclerosis?
Family history can make a difference. People who have a close relative with MS, like a parent or sibling, have a higher chance of developing it compared to those with no family history due to their genetic predisposition.
Should children of a parent with multiple sclerosis consider genetic testing?
Currently, routine genetic testing for MS risk is not recommended. There is no single gene that predicts who will get MS, and testing does not give clear answers or useful prevention steps to determine MS risk in families.
What is the risk of inheriting multiple sclerosis if a sibling has been diagnosed?
If a sibling has MS, the risk increases compared to the general population. While most people have a risk of about 1 in 333, siblings of someone with MS have a higher chance, though it is still low for most families. More details are available from the National MS Society.
Are certain individuals at greater risk for developing multiple sclerosis due to genetics?
Is there a genetic component to multiple sclerosis? Some people do have genetic factors that make them more likely to develop MS. Over 200 genes may affect risk, but each gene only has a small effect.
How does having a relative with multiple sclerosis influence a person’s risk?
Having a close relative with MS raises a person’s risk but does not guarantee they will get the disease. Genetics combine with other factors like location, sunlight, and infections.
What genetic factors contribute to the development of multiple sclerosis?
MS is linked to many genes, not just one. These genes are involved in the immune system. While over 200 genetic variations have been found, none alone can cause MS.
Does multiple sclerosis run in families?
MS does not follow simple rules of inheritance and is not directly passed down from parents to children. However, it can run in families more than would be expected by chance alone.
Who is at high risk for MS?
People with a family member who has MS, those of Northern European descent, and those who live farther from the equator have higher risks. Women are also more likely to be diagnosed than men. Other factors like low vitamin D levels and certain viral infections may also play a role.






